Pharmacotherapy: Treating Mental Disorders
 Flickr by Erin
Flickr by Erin
Mental health has received a lot attention in recent years. We have become increasingly aware of our mental well being and stigmas by talking about the diagnostic methods (DSM-V); however, there should also be more discussion on post-diagnostic treatments when one is diagnosed. There are two main popular treatments of mental disorders: pharmacotherapy and psychotherapy. Essentially, pharmacotherapy is using medication to counter mental disorders; psychotherapy consists of “talk” sessions in which a trained professional will address one’s personal problems. Although the amount of researches studying different kinds of mental disorder is increasing, there are still a lot of unknowns in this field that raises skeptical views about the treatment options for mental disorders, especially for pharmaceutical drugs targeting mental disorders, on whether they are effective or how they are prioritized.
Firstly, some argue that psychiatric drug research and developments are not very well studied. Pharmaceutical companies tend to overrate the positive effects of the drug treatment and then selects a handful of clinical trials to be published, hence misguiding the patients about the success rate of the drug. In a study conducted in 2008, Turner and his colleagues found out that “[a]mong 74 FDA-registered studies, 31%, accounting for 1449 study participants, were not published”(Perlis et al., 2005). The findings also show that half of the studies that were perceived positively by the FDA are published, while 11 of them “conveyed a positive outcome” even when the FDA questioned their results or viewed them as having negative outcome. Adding to that, 94% of the published literature has successful trials while FDA has only concluded 51% of the publications as having successful trials. There is a striking difference in presenting trials between the published literature and FDA’s analysis, which suggests an inclination of the pharmaceutical companies to selectively publish their results. This selective bias imposes a risk to the industry and particularly to patients. Disclosing drug developments that only have good results inevitably misguide medical professionals and the patient; lack of research behind potential backlashes of a drug could easily cause medical professionals to overestimate drug’s success and oversee the negative impacts the drug may bring to the patient. We, as human, learn through mistakes. Without publications that point out bad outcomes of the drug of interest, this can hinder the rate of improving and developing drug in the pharmaceutical industry.

Additionally, the side effects associated with psychiatric drugs can negatively affect the patient’s quality of life that contradicts with the primary principle of medicating the patient, to improve one’s everyday life. Building up on the reluctance of pharmaceutical industry to release such information, patients are generally not very well informed of the side effects a psychiatric drug might have. Also, the development of psychiatric drugs is relatively new unlike other drugs like aspirin, which has been under intensive research – positive and negative. Patients diagnosed with different kinds of mental disorder can have different side effects; some common ones are: nausea, dizziness, and dry mouth. These undesirable side effects are caused by the “lack of specificity” in modern psychiatric drugs, as we still largely don’t fully understand the “natural law of the underlying development of psychopathological symptoms”, hence have limited knowledge in prescribing an optimal drug treatment for patients (Henn, 2001). Like Tylenol which relieves us from nasal congestion during a cold but doesn’t target the source of the cold, psychoactive drug works to provide relieving symptoms, such as reduced hallucination, which is a manifestation of the disorder but not the source itself. Therefore, even if the drug gives relief from the actual disorder, it also introduces another type of “symptoms” that can bring down a patient’s life quality.
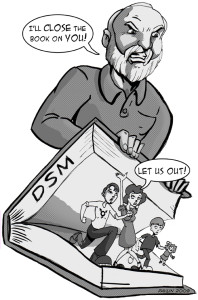
Another issue arises due to the current diagnostic method, DSM-5. This particular diagnostic test has received a lot of attention related to the difficulty in distinguishing misbehaviours from an actual sign of a mental disorder, such as ADHD. The diagnosis guideline for professionals is ambiguous and “these concepts are virtually impossible to define precisely with bright lines at the boundaries,” as confessed by Allen Frances, the lead editor of DSM-IV. The ambiguous nature of DSM can be risky. Patients can be easily misdiagnosised, thus receiving medications that they do not need. Additional to the heavy marketing from the drug industry that sugarcoats the success of psychiatric drugs, professionals maybe have a higher tendency to prescribe them to patients to relieve their symptoms, which may turn out to be unnecessary and could physiologically cause harms. Unfortunately, there is an over-reliance on prescription to treat patients rather than having comprehension therapies, which is alarming because the patients may not require them. Therefore, we should not treat psychoactive drug as the sole bible on treating mental disorders.
Furthermore, some patients develop treatment resistance, by questioning the effectiveness of pharmacotherapy. Since mental disorders can last a long period of time, patients can develop treatment resistant mental disorders during the course of treatment. A common example is refractory schizophrenia in which 30% of the patients in a study had developed resistance. Not only does this raise doubts on the drug’s efficiency, it also questions the justification of the methods that counteract the resistance such as increasing dosage or switching to a new medication. It is uncertain whether the other medications work. Also, if the psychoactive drug alternative did not work, is increasing dosage of the original medication the only way out? Treatment resistance mental disorder seems not to differ as much as antibiotics resistance diseases. Increasing the dosage or switching medication could possibly introduce new side effects or worsen them. Hence, instead of prioritizing pharmacotherapy over psychotherapy, we should focus on and appreciate more psychotherapy, such that patients do not solely rely on psychoactive drugs but also have talk sessions to understand more about what their disorders really entail. Merely depending on drugs that could be ineffective after a period of time is not the best long term solution in a battle against mental disorder.
Psychotherapy is beneficial for patients to develop a cognitive control over their disorders. The therapy is highly personalised, in which patients may think the therapists or psychiatrists are more interested in them as individuals rather than treating them as patients with symptoms. During talk sessions, patients are encouraged to talk about their problems that therapists help by giving advice or analysising patterns that may trigger the occurrence of symptoms. This can help the patient to understand more about their manifestation of their symptoms, which can help to reduce anxiety or know better how to manage when symptoms hit hard. This encourages patients to have a “I can do it” mentality – stronger cognition; it gives patients back a sense of control and self-reassurance. This can be beneficial in fighting mental disorders in a long run.
In conclusion, we should be more cautious about pharmacotherapy as the positive results from drug studies could be overrated, mis-prescribed, and potentially cause side effects despite treating the symptoms of a mental disorder. Pharmacotherapy should also be treated in parallel with psychotherapy since drug efficiency can vary over time. Rather than only focusing on relieving patients from their symptoms, professionals should give more credit to psychotherapy for helping the patients build a stronger mind control over their own disorder and targeting the source of their mental disorder rather cognitively than chemically.
Interested in learning more about Psychotherapy? Click on the link to learn more!
References
- Cuijpers, P., Berking, M., Andersson, G., Quigley, L., Kleiboer, A., & Dobson, K. S. (2013). A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 58(7), 376-385.
- Desjardins, L. (2013). Psychiatric drug prescription up in Canada. Retrieved from http://www.rcinet.ca/en/2013/07/28/psychiatric-drug-prescription-up-in-canada/
- Frances, A. (2009). A warning sign on the road to DSM-V: Beware of its unintended consequences. Psychiatr. Times Psychiatric Times, 26(8), 1+4-5+8-9.
- Henn, F. A. (2001). Contemporary psychiatry. Volume 1, Volume 1. Retrieved from http://dx.doi.org/10.1007/978-3-642-59519-6
- Perlis, R. H., Perlis, C. S., Wu, Y., Hwang, C., Joseph, M., & Nierenberg, A. A. (2005). Industry sponsorship and financial conflict of interest in the reporting of clinical trials in psychiatry. The American journal of psychiatry, 162(10), 1957-1960.
- Self, W. (2013). Psychiatrists: the drug pushers. Mental Health. Retrieved from http://www.theguardian.com/society/2013/aug/03/will-self-psychiatrist-drug-medication
- Sen, S., & Prabhu, M. (2012). Reporting bias in industry-supported medication trials presented at the American Psychiatric Association meeting. Journal of clinical psychopharmacology, 32(3).
