The “Ozempic Craze”: Intersections Between Healthcare Access and Societal Body Standards
 “Male Gaze” by Tyler Hewitt is licensed under CC BY-NC 2.0
“Male Gaze” by Tyler Hewitt is licensed under CC BY-NC 2.0
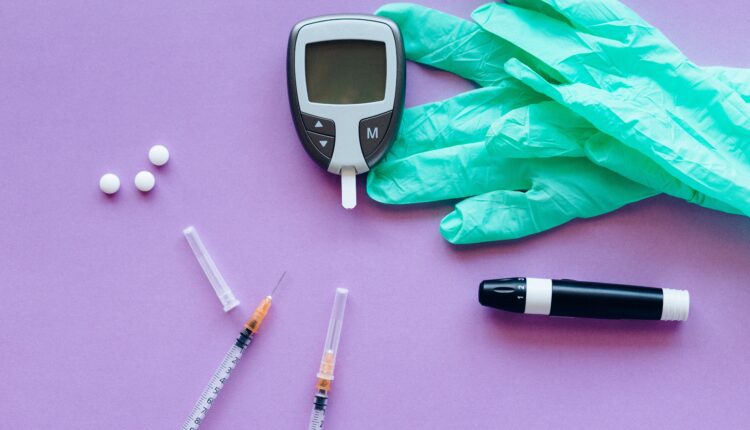
The brand name Ozempic has become a trending topic across social media and doctor’s offices. Approved by the FDA in 2015, Ozempic was initially developed as a Type-2 diabetes drug by Novo Nordisk. The active ingredient, semaglutide, increases insulin production and reduces glucagon, lowering blood sugar levels for those with diabetes. It can also create a lasting feeling of fullness, decreased appetite, and increased energy expenditure, ultimately expanding the likelihood of fat-burning during rest periods.
This unanticipated effect has gained Ozempic notoriety as a rapid weight loss remedy for the dieting community. Although there has been a growing body positivity movement in recent years, Ozempic has become the latest it drug for people to attain a desirable body standard. On TikTok alone, videos under the hashtag #myozempicjourney have amassed over 600 million views and counting, where users document their weight loss journeys on the drug, depicting drastic results. The drug has become so popular that it has caused mass shortages across the United States, prompting Novo Nordisk to develop Wegovy, an injectable prescription medication approved in 2021 by the FDA as an obesity treatment. Wegovy uses the same active ingredient as Ozempic – semaglutide – but at a higher dose. Neither drug is a cure-all, however, and they come with significant drawbacks. Semaglutide is known to cause side effects ranging from nausea and diarrhea to kidney failure, pancreatitis, and thyroid tumours. Ozempic and Wegovy are quite expensive, costing upwards of $1000 US per month, and for the most part, not covered by insurance in the United States. Despite these factors, the American public has not been discouraged from trying Ozempic for weight loss purposes.
Diet pills are nothing new; people have been searching for a magic drug that can shed pounds away for centuries. Amphetamines, dinitrophenol, ephedra, and rimonabant are all examples of drugs used ubiquitously for weight loss. What makes Ozempic more attractive than the rest, is that, one, it is legal (for the time being), and two, it is being heavily marketed through social media platforms, including TikTok and Instagram. Ozempic and Wegovy have become household names in the span of a year, leading to a mass following that simply would not be possible in a time without social media. This has led many public health experts to question whether the drug is something to be concerned about. Indeed, the rise of Ozempic has brought forward several discourses surrounding body standards, pharmaceutical ethics, and society’s relationship with over-the-counter drugs.
On one hand, developing a drug that can help those with obesity should be a cause for celebration. Obesity, much like diabetes, is a chronic condition that can increase the risk of heart disease, liver disease, and cancer. While policy options that focus on improving people’s access to fresh produce and making cities more walkable are important preventative measures, they are not enough to treat the 40% of Americans diagnosed with obesity. Drugs like Ozempic can have a widespread impact on the lives of many struggling with obesity, much like they can ameliorate the lives of those diagnosed with type-2 diabetes. For one, Ozempic does not increase the risk of cardiovascular disease, contrary to other drugs for obesity and type-2 diabetes. On the other hand, the real problem lies in the implementation and distribution of Ozempic. The reality is that obese people and diabetics are not the ones causing the semaglutide shortage.
Social determinants of health play a large role in this conversation. Obesity is closely linked with low socio-economic status, as racial minorities and low-income individuals have the highest rates of obesity. Given this fact, it is unlikely that clinically obese people are consistently purchasing Ozempic for $1,000 a month. Instead, affluent influencers and celebrities have been spearheading the drug’s craze, driven by a vain desire to obtain impossible beauty standards, rather than seeking treatment for a chronic condition. The Ozempic craze has also been taking place simultaneously as the “heroic chic” look and thinner bodies become “in” again, highlighting the societal tendency to categorize body types into trends. This puts into question how strong a foundation the body positivity movement has had, and whether we ever stopped caring about what size we are.

Access to Ozempic is hard to come by, but health professionals have become lenient with who they deem fit for obtaining it. This was highlighted in a New Yorker article where journalist Jia Tolentino was able to attain an Ozempic prescription for post-pregnancy weight loss without any hesitation or questions asked, despite not being diabetic or obese. Those who are unable to easily receive prescriptions – whether it be for medical or aesthetic reasons – seek out a variety of other off-brand options or decide to turn elsewhere, including Canada, where it costs a fraction of the price. However, the situation is so dire that B.C. Health Minister Adrian Dix is asking the provincial and federal health regulators to investigate whether Canadian pharmacies have prescribed thousands of Ozempic prescriptions to Americans in 2023.
The unnecessary Ozempic prescriptions to individuals who are not diabetic nor obese highlights the stigma against larger-bodied people from the medical community. Fatphobia in the medical community exists far beyond Ozempic prescriptions, with many larger-bodied individuals recounting prolonged diagnostics and discrimination in the doctor’s office, pushing them to lose weight. Ozempic and Wegovy serve as yet another tool doctors can push onto individuals, rather than take the time to listen to their patients. The mass prescriptions of Ozempic to those for whom the drug is not intended are dangerous and unethical, considering there is little research on the long-term effects of semaglutide on healthy individuals.
With negative biases towards fat people on the rise, the Ozempic craze raises concerns about just how far we as a society will go in our pursuit of thinness. The simultaneous resurgence of unnaturally thin ‘heroin chic’ bodies have naturally progressed alongside the popularity of Ozempic. It is unclear what direction the current situation will take. Because of our societal body standards, the Ozempic craze has left many without the medication they need. Ozempic has highlighted the intersection between prescription drugs, accessibility, medical inefficacy when providing patients with medication they actually need, and the overarching desire for thinness. The affluent set standards that are unattainable without external intervention, such as drugs or plastic surgery. This leaves the rest in a constant cycle of trying to achieve body trends, no matter the cost. Although the desire for thinness and body trends are not new, the phenomenon has reminded us that despite a growing body positivity movement, body standards and the desire to have the “right” figure continue to influence our consumption habits, even medication.
“Male Gaze” by Tyler Hewitt is licensed under CC BY-NC 2.0
Edited by Derya Ekin.
