What does free healthcare look like?
Financial transparency within Québec's healthcare system: a closer look at the data
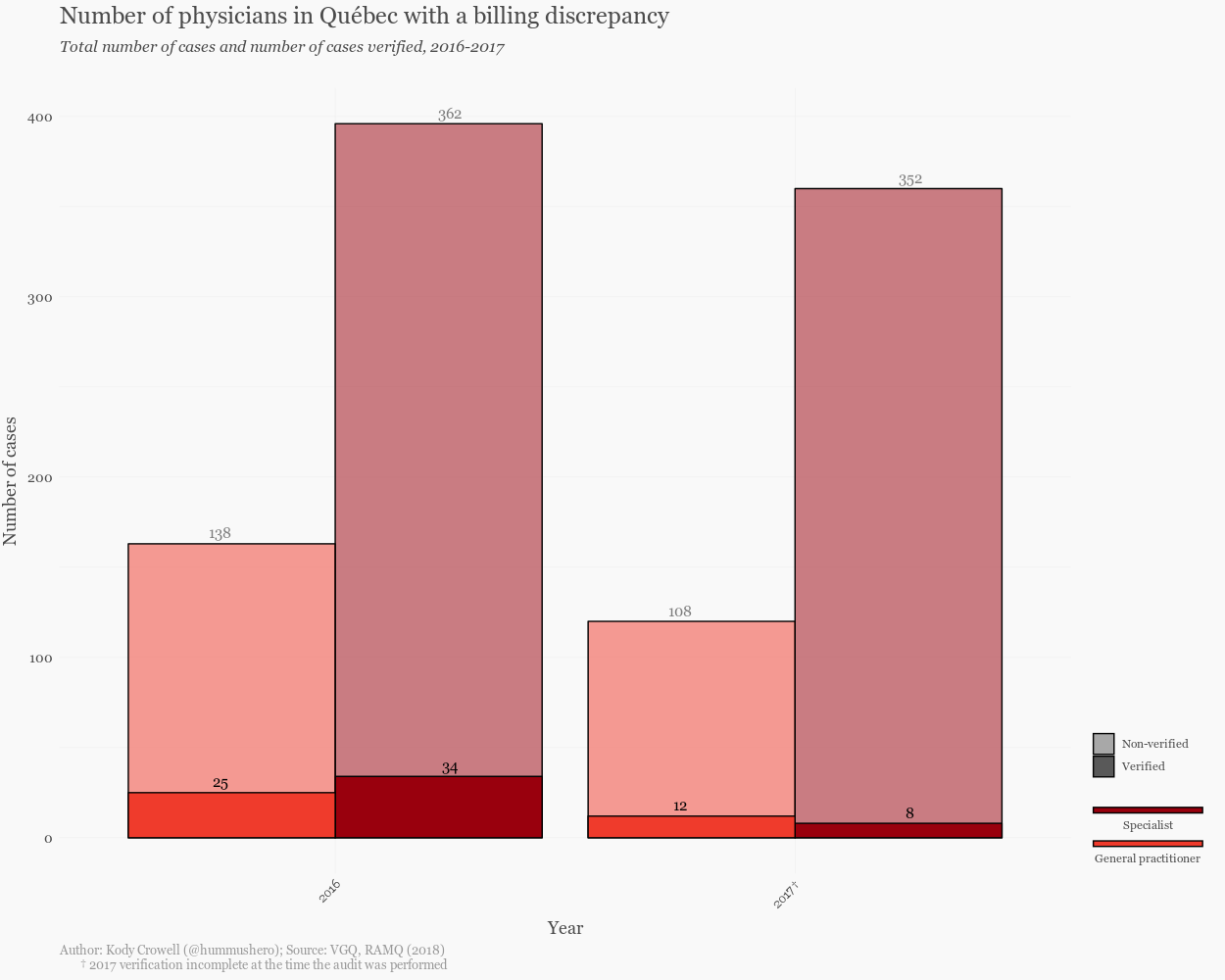
On November 30, 2018, the Auditor General of Quebec (Vérificateur général du Québec, hereafter referred to as VGQ), released a new report to the National Assembly of Québec outlining the continuing practice of overbilling by physicians. The Régie de l’assurance-maladie (RAMQ) is mandated under section 64 of the Health Insurance Act to periodically check whether the services charged were actually rendered. However, RAMQ’s efforts have been practically non-existent. In 2014, only 2% of physicians had their billing history analyzed, usually for one specific act. Between 2017-2018, at the time of VGQ’s analysis, RAMQ had barely scratched 5% of the cases where billing gaps were found. In 2016, only 12% of cases were verified.
Public trust in physicians has been declining over the past few years and it’s no surprise. The commodification of the medical profession and overbilling are just a few of the spectres that haunt the Canadian healthcare system. Lags in verification of billing practices mean less transparency for Canadian citizens, and physicians themselves do little to assure the public that their funds are in good hands: the oligarchic medical colleges keep a tight grip on their data. In some cases, this has translated into legal battles: the Ontario Medical Association (OMA) has turned to the Supreme Court of Canada for an appeal to keep the names of their top billing doctors a secret. In British Columbia, one auditor’s independent investigation into the billing practices of a single doctor reaped a repayment of over $2 million dollars.
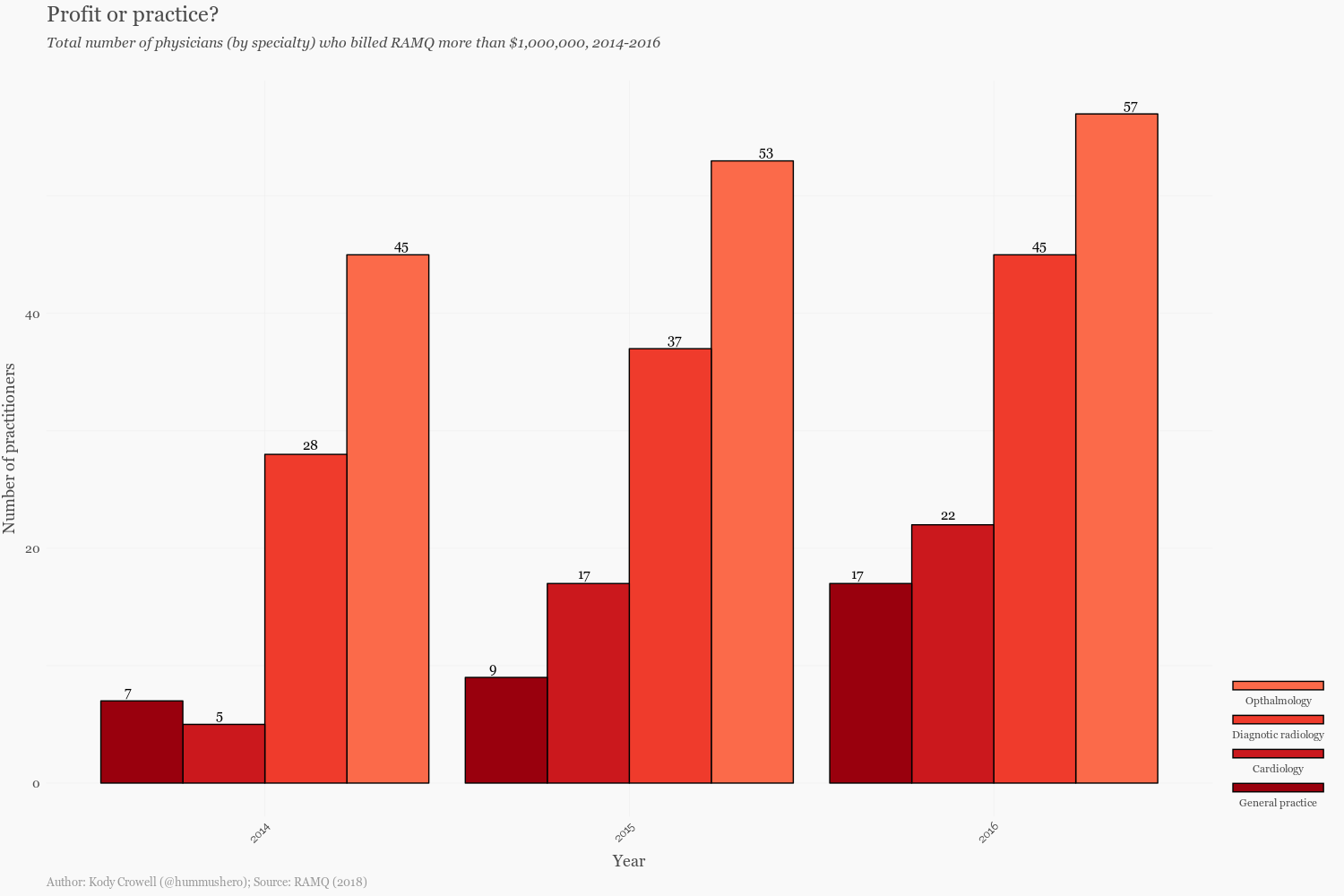
RAMQ’s surveillance has been expanded to include cases where doctors exhibit a billing gap or where doctors charge the organization more than $1 million dollars annually. By investigating 184 doctors in 2016, RAMQ was able to retrieve roughly $10 million dollars in overpayment. Of course, some medical specialties are naturally more expensive than others: drugs, supplies, staff required, and medical equipment all contribute to the variability in the costs of healthcare. According to data provided by RAMQ, ophthalmology, diagnostic radiology, cardiology, and general practice were the specialties in which the largest number of physicians charged the organization more than $1 million in 2016 (see figure below). One must ask how these doctors’ billings accumulated so quickly and to what extent we find these practices unwarranted.
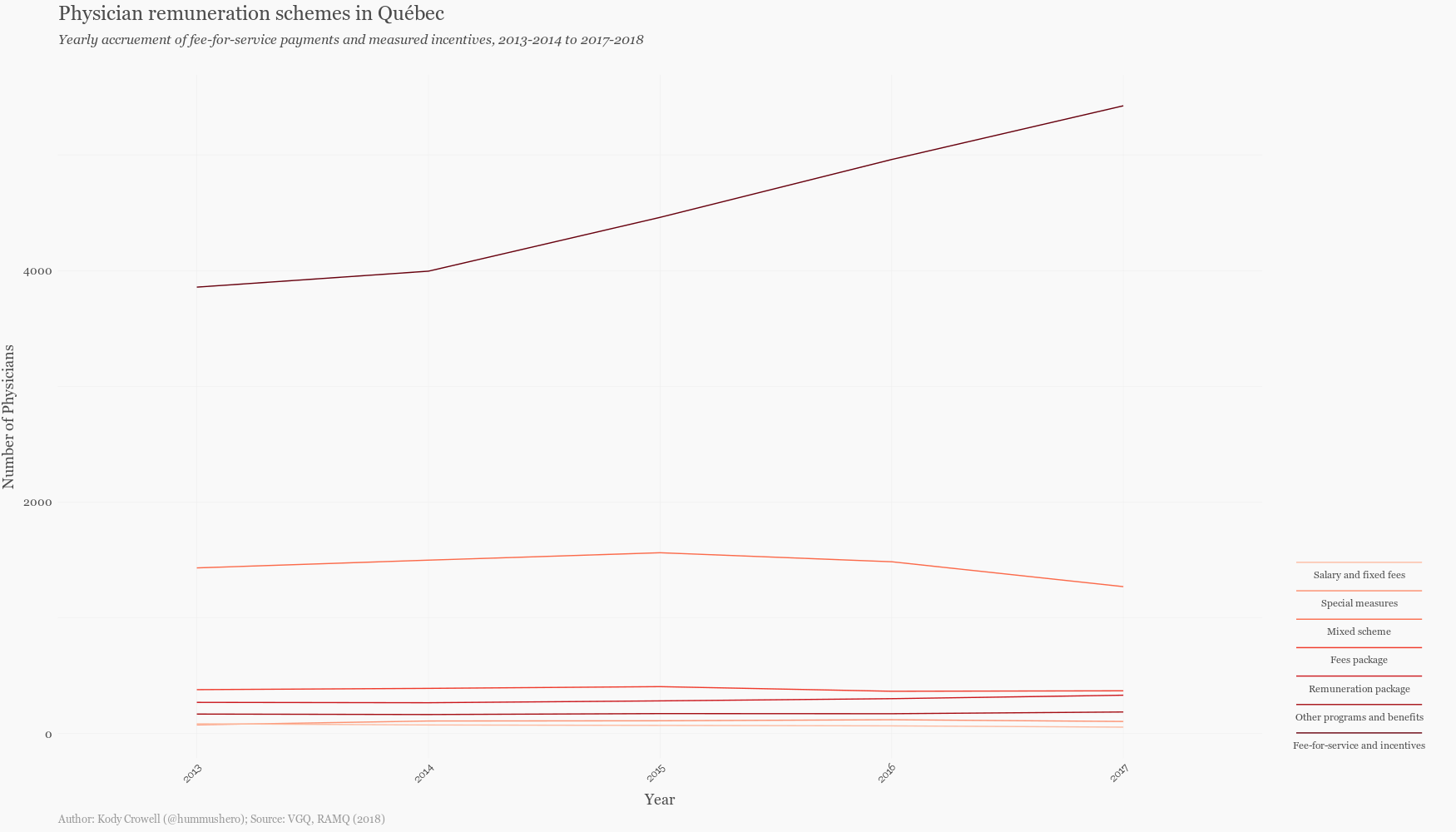
It is also important to discuss the remuneration model from which these billing practices stems. The healthcare system in Québec and the rest of Canada follow a fee-for-service (FFS) scheme, where physicians are paid for each service they perform. There are more than 21,409 physicians enrolled in the RAMQ, constituting a 70% FFS population as of 2016. This number has been steadily increasing over the last five years.
How does this remuneration model affect physicians’ quality of care? It has been noted that a fee-for-service scheme can encourage physicians to neglect the financially unrewarding and time-consuming work of chronic disease management and preventative care, both of which are critical if we wish to address our rising healthcare costs. Moreover, some have argued that fee-for-service models cause physicians to value quantity over quality of care and that specializations with exorbitant incomes tend to attract those who are more interested in status and wealth, rather than a genuine desire to serve. Some doctors in Canada have been found to illegal double billing of the government and patients. Others have found similarly dubious means of maintaining their gross income through independent medical examinations (this goes well beyond the stringent sheltering of doctor malpractice history). In Québec, accessory fees — or the practice of extra billing on healthcare services including those already covered by RAMQ — was so widespread that the government eventually passed a ban, claiming that physicians who don’t follow the new rules will face penalties. The practice has not stopped.
Physician expenditure is a leading driver in healthcare costs, putting a massive strain on provincial budgets. Reluctance to different forms of remuneration is well-observed in the Canadian context. Although physicians do seek remuneration from alternative payment plans, fee-for-service remains the most popular means of income for doctors. Accountability within this realm varies by province: British Columbia releases annual statistics on fee-for-service payments to practitioners, whereas the OMA continues to dismiss calls to disclose physician billings. Keep in mind that despite jurisdictional differences in healthcare systems, the money still comes from the public’s purse.
Transparency is critical to ensuring that our institutions are held to a high standard. Accountability and openness demonstrate organizations’ commitment to protecting the public. Yet in Québec, the numbers show a clear divergence from this standard. So why the lackluster performance by RAMQ? The VGQ offers some insight: although RAMQ has reviewed and streamlined its analysis process, the tools used to analyze billings were focused only on physicians whose billing profile deviated from the average observed in their colleagues. The RAMQ thus failed to consider the cases where the inappropriate use of a service fee code would be widespread in practice. Moreover, while RAMQ has taken steps to broaden the scope of its control over non-FFS methods of compensation, the effects of these actions have not yet demonstrated any positive impact.
Canadian exceptionalism regarding healthcare is well-documented. Indeed, without any exposure to actual the costs of medical care, most Canadians are willing to laud their system as free. This is often presented in contrast to the United States, whose healthcare system is at best a patchwork system of varying insurance schemes bankrupting the nation. However, doctors in the United States are still held on tight leashes by administrations who strongly value their patient assessment-of-care surveys. But in Canada, doctors are self-regulated, the consequence of which is an “endemic secrecy.”
Healthcare in Canada is far from free and not as universal as it is often purported to be, and it is certainly not transparent. Leaving aside the fact that dental care and prescriptions are not publicly funded, Canadians have no easy way to actually calculate how much of their tax dollars are directed toward healthcare, since healthcare is funded by general government tax revenue and not by a dedicated health insurance tax. Compared to other developed countries, Canada performs poorly, especially in terms of access, equity, and health outcomes. If we spent as much as we do on doctors’ salaries on developing a transparent and sustainable healthcare system, perhaps we would see these rankings change.
Thanks to my dear friend and colleague, Arisha Khan for her help with this piece @arisha_khan1. To view the VGQ’s full report, click here (French only). All plotting code is available on the author’s GitHub, @eisengrim. For more on health and data, follow the author on Twitter: @hummushero.
Edited by Sarie Khalid
